Free E-Book – 2022 Nursing Shortage Statistics
An Overview of Staffing Trends
We have collected research-based statistics on the ongoing nursing shortage and compiled predicted employment trends for the healthcare industry. Below is a short summary of our findings and the topics covered in depth within this E-book.
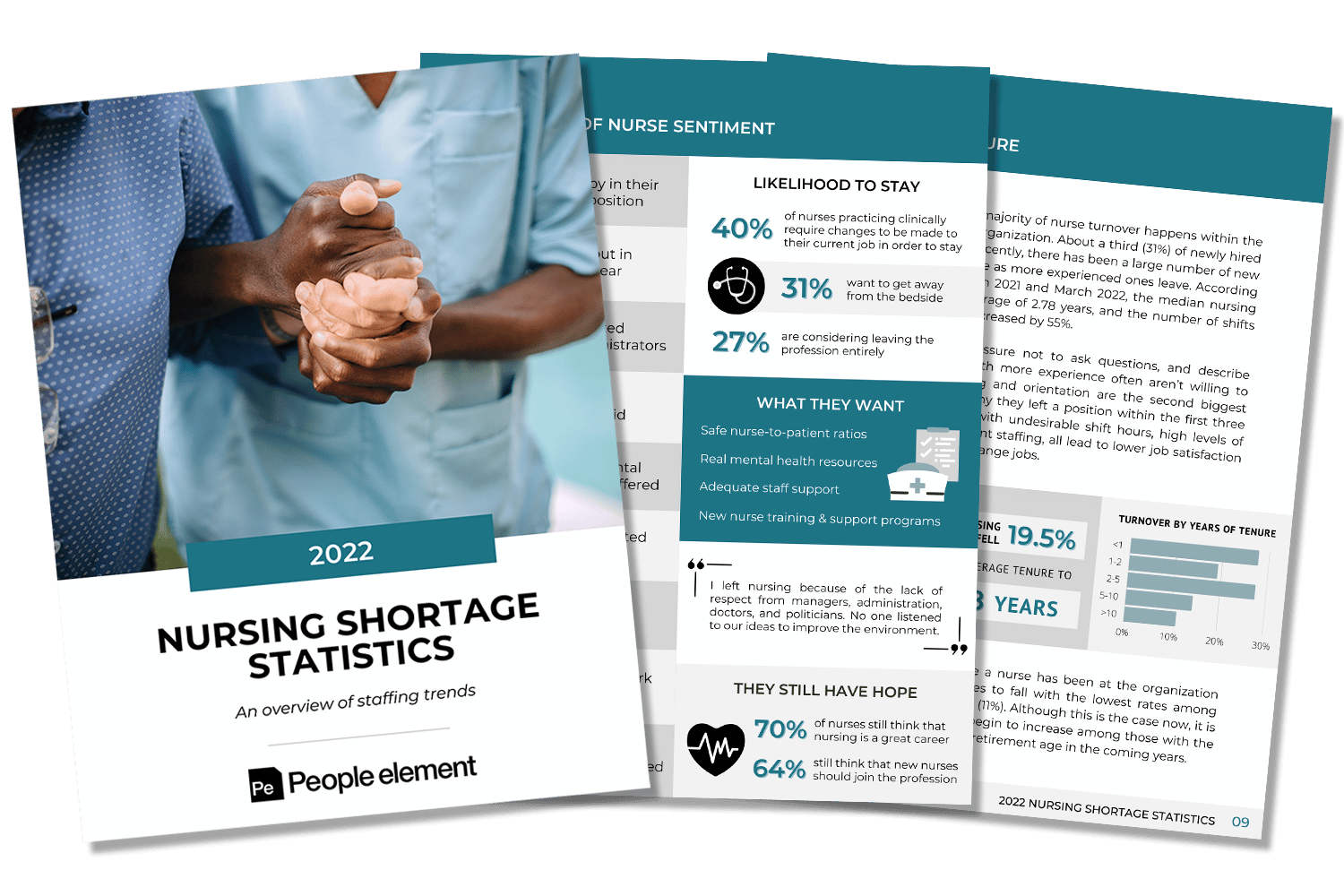
Overview of Nurse Sentiment
Nurses are working through extremely difficult times, facing high rates of burnout and stress as they navigate understaffed units. According to a 2022 report, only 12% of nurses feel happy in their current position and 87% felt burnout in the past year. The majority of nurses (70%) still think nursing is a great career but they would like to see changes made, like adequate staff support and new nurse onboarding programs.
Growing Demand for Nurses
To say that nurses are in high demand would be an understatement. The
demand for nurses has been steadily growing over the years and is
expected to continue. According to the U.S. Bureau of Labor Statistics,
about 276,000 additional Registered Nurses will be needed from 2020 to
2030 bringing the total RN employment from 3,080,100 in 2020 to 3,356,
800.
Aging Nurse and Patient Populations
By 2030, according to the U.S. Census Bureau, more than 20 percent of U.S.
residents are projected to be age 65 and over, compared to just 9.8 percent of the population in 1970. This means an increased demand for healthcare and skilled nurses to accommodate the aging Baby Boomer population. Nurses are no exception to the increasing number of retirement-age individuals. It is predicted that over 1 million nurses will retire in the next 10 years.
The Nursing Shortage Over Time
While management in every industry wants to avoid turnover, job vacancy
issues in the healthcare industry are more than an inconvenience—they
can be a life-and-death matter. The nursing shortage has been increasing
over the last decade and skyrocketed in the past few years due to the
COVID-19 pandemic. According to a 2022 report, in 2020, the RN turnover rate was 18.7%, with an average job vacancy rate of 9%. In just one year the turnover rate jumped 8.4 points, hitting 27.1% in 2021.
Most Severe Shortages Expected by 2030
The nursing shortage is expected to continue over the next ten years. Based on projected supply and demand numbers, the following states are predicted to have the largest shortages by 2030: California (-44,500), Texas (-15,900), New Jersey (-11,400), South Carolina (-10,400), and Alaska (-5,400).
Cost of Nursing Turnover
The longer a nursing position is vacant, the more costly it becomes in terms of overtime, and staff burnout. The average cost of turnover for a bedside RN is about $46,100, ranging from $33,900 to $58,300. It’s ultimately more cost-effective to understand what would enhance engagement and job satisfaction within the organization to attempt to lower turnover than it is to pay the price of losing skilled, trained nurses.
Turnover By Tenure
Turnover is happening quickly and frequently among newly hired nurses. Research indicates that the majority of nurse turnover happens within the first year of service with an organization. Turnover begins to decrease after about 5 years with the organization and hits its lowest point after 10 years. As more nurses begin to retire we will start seeing turnover trend upwards among those with the longest tenure.
Impact on Quality of Patient Care
High nurse turnover and vacancy rates affect access to healthcare and
impact the level of care patients receive. Several studies suggest a correlation between appropriate levels of RN staffing, safe patient care, and mortality rate.
Nursing School Capacity Issues
Nursing schools are also being impacted by the nursing shortage, limiting the number of students they are able to take on due to a lack of faculty. According to a report from the American Association of Colleges of Nursing, in 2020 over 80,000 qualified applicants were turned away from nursing baccalaureate and graduate programs.





